"My Changes, Are They Reversible?" Yet More Chatting About HRT, With Lola Pellegrino
Previously: A chat with Jules Gill-Peterson, author of Histories of the Transgender Child, about “microdosing” and HRT.
Lola Pellegrino is a nurse practitioner and HRT provider in Brooklyn. She used to write on body topix for the Hairpin and Rookie (double RIP).
DANIEL: Lola! After I published my conversation with Jules last week, you mentioned having thoughts on the subject as a nurse practitioner in reproductive health, and very kindly agreed to answer some follow-up questions.
Contingent upon the widespread interest “microdosing testosterone” is, I think, some general sense that testosterone is “stronger” than estrogen, that its efficacy has to be carefully bridled and managed from the outset, that doesn't seem to be true in the other direction. “Testosterone is really powerful” is something I’ve heard from a number of trans people and healthcare professionals; I don’t think I’ve often heard anyone say “Estrogen is really powerful,” at least not in the same way. Are you familiar with this in your own work? Do you have a sense of what patients might be trying to communicate when they say something like this?
LOLA: Ok!!! Yes!!! I hear this constantly. I want to say I am cis and a clinician so I hope to speak from that viewpoint only!!!!!!! In the exam room but all the way over here!!
T POWER > E power is a Real Thing that affects both patients and clinicians. Everybody. To start with the most concrete answer — on an individual basis, yes, there are some permanent, externally perceptible features that can happen in the first couple months of taking T. The way this breaks down for me as a provider is, say I have a patient uncertain whether or not to start T now, during our ‘informed consent discussion’ I’d ask, “There is a chance that no matter how low your dose is, when you come back for your three-month appointment with me, you could already have your voice drop, some bottom growth, and maybe a little facial hair. Is that cool, or is that a dealbreaker?” If they say it’s cool, then it’s cool. There is no corresponding estrogen disclaimer; but like you’ve mentioned and we’ve discussed, it’s not because estrogen therapy doesn’t change a person in many ways, it’s often just a lot of internal stuff at first, changes that are not as permanent AND visible to others in a way as early as with T.**
**Re: fertility: for both T and E, we know so little about how and when and what factors will impact the fertility of someone on HRT — it’s not a given but it could also theoretically happen any time — we make sure to talk about the possibility of reduced fertility from the jump.
DANIEL: I’m so curious about this! I realize I might fall into a corresponding error and try to overcorrect by arguing that T and E have basically identical effects or operate on a identical-yet-antithetical schedule, so I want to maintain a wary distance from my own bias, but it seems to me that there is a similarly-strong basis for saying to a patient, “There is a chance that no matter how low your dose is, when you come back for your three-month appointment with me, you could already see changes in your body and facial hair growth, as well as development of breast tissue,” for example. This idea of estrogen working imperceptibly and “behind the scenes” or “below the surface,” working in Cowper’s “mysterious way [her] wonders to perform” while testosterone works externally/obviously/immediately/permanently, seems to me to fall prey to the same problem. “Testosterone therapy often results in noticeable bottom growth within the first three months, even at a low dose,” for example, strikes me as a (relatively) neutral piece of information to pass along to a patient considering HRT; “Testosterone produces a lot of immediately-visible effects, so I’m legally obligated to warn you in a way I’m not obligated to warn someone considering estrogen/anti-androgens” strikes me as a step beyond, a categorical claim about power, efficacy, and social legibility.
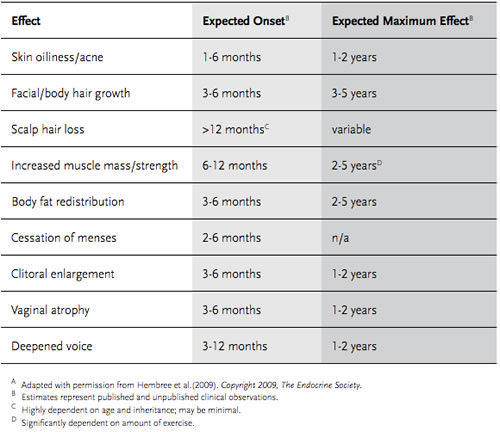
LOLA: This is a tough and nuanced point so I’m going to bring out…….. charts from the endocrine society standards of care!!!!!!!
Here’s T:
And here’s E:
Let’s take the permanent changes you mentioned. Onset for bottom growth, voice changes are 3 months; comparatively, onset for breast growth and decreased testicular volume are...also 3 months. Anecdotally I’ll see both of those start earlier and/or be reported to me as starting earlier. However, bottom growth and voice changes peak at 1-2 years, and breast growth/testicular changes are 2-3 years. This is a chart from a guideline and not reported experiences, but I think the pace differential is significant in terms of why I’d say one thing and not the other.
I should say, this is me speaking as an individual provider who basically wants you to have the hormones u desire ASAP (unless they’re going to immediately kill you). I feel a responsibility to make HRT accessible through informed consent to my (fully informed and consenting) patients because the decision is theirs and I trust them to make it; withholding the scrip because they didn’t convince me (or some shit??? Idk why people gatekeep, really) is denial of someone’s bodily autonomy and I think unethical, especially in consideration of a transphobic medical system.
DANNY: Honestly, my first response, seeing this, is “What a relief! When I went for my first informed-care appointment back in 2017, the standards of care packet was from 2009, so at least they’re making some updates.” And while I do take your point about the difference between an expected onset of 1-3 months as opposed to 3-6 months, the T & E timetables seem to have more in common than otherwise — that is to say, they don’t appear to act as “equal and opposite forces,” but with many broadly similar ranges/scopes/interventions.
LOLA: More abstractly, people sometimes view testosterone HRT as obliterating or dominating their pre-existing selves in a way that estrogen wouldn’t. An example: often, during an intake when I ask people if they have any worries about the process, people starting T often express those in terms of “I don't want to turn into X [a Man/a scary Man/my father/what have you]”; people starting estrogen are more often worried that it won’t be “enough” to meet their goals. As Jules said: there don’t appear to be similar widespread concerns “What if I'm too much of a woman?”, at least not expressed to me in this context.
And then even more abstractly, from a biomedical perspective only, I think the most interesting thing is like everything else, “female hormones” and “male hormones” dimorphism is bullshit lol. We all have all of them. In lieu of a genetic/congenital variant, every human is born with the capability to produce and use testosterone, estrogen, and progesterone. There are roughly equal amounts of all three until natal puberty hits and T or E become dominant, depending on what you rolled gonad-wise (100% of the time I think of this as an RPG character creation process). But everyone needs all three even if it’s a small amount (for instance, many of my estrogen HRT patients are surprised that the therapeutic goal is for double-digit suppressed T levels, and not totally annihilated zero; but a T level of zero below suppression doesn’t accelerate changes and causes a lot of cognitive/energy problems.)
DANNY: I was rather struck by the variations on “normal levels” when I started T, too – I believe my provider said anything between 400-1200 ng/dL of total testosterone was safe/effective. Which is part of why I’ve found myself so surprised by more recent claims about “microdosing,” I think, since the “standard range” is already quite wide!
LOLA: Yup. As a general rule, we go by how people feel and not just what the numbers say because the “safe” range is wide and hormone-level testing is arbitrary and fickle. Even if they’re not on HRT, someone’s T/E levels can be affected by a million factors INCLUDING age, the time of day, if they have ovaries, when they are in a menstrual cycle, other medications, what lab they went to, the gender marker the lab they went to saw….I mean, beyond making sure you’re not in clinical danger, labs are a vibe. They are simply a vibe, and these vibes are but one part of the puzzle.
And THEN it’s so much more complex than just a binary T or E dominance because the endocrine system is many, many entities in constant close adjustment with and to one another. For instance! Testosterone and estrogen and progesterone all share a precursor (building block) called pregnenolone, and progesterone itself is one of testosterone’s precursors. Someone with testicles requires progesterone for sperm maturation. In someone with ovaries, high levels of T can convert back into E through a process called aromatization. And then estrogen and progesterone can work together or against one another...basically frenemies? Estrogen and progesterone come to the party together and estrogen gets drunk and mouthy and progesterone is like “Shhh, be quiet.” I’m just saying. Lots of interactions here.
Further Vibes: Estrogen is powerful!!!!
DANNY: Thank you for saying so! She deserves some credit! She’s a strong woman! People sometimes talk about estrogen the way medieval theologians talked about women, like it’s the ghost of testosterone or something, God’s first pancake that he messed up before getting it right with Boy Juice: The One That Works.
LOLA: I think another manifestation of the widespread belief in T’s Ultimate Strength delayed some clinicians (certainly me) into considering estrogen monotherapy (estrogen with no T-blocker) as an option. The way I originally learned it, someone’s testosterone has to be heavily suppressed in order for estrogen’s effects to bloom. And there are certainly some characteristics that give people dysphoria that blocking T is the most direct route to minimizing — body hair and libido, for example. Thinking about changes very generally; not just “feminizing” and “masculinizing” but also “de-masculinizing” and “de-feminizing” (sort of like a Cartesian grid vs. a linear spectrum) But although it’s still pretty murky, estrogen is really the engine in many ways. And in many people, taking estrogen can eventually suppress T on its own.
DANNY: This is really interesting! I want to stress at this point that I’m interested in decoupling value claims like “T is powerful” (and the implicational relationship that “E isn’t very powerful and needs a perfectly-tidied room and a few good friends by her side before she can get to work) from specific issues like “T will likely change the sound of your voice” and “E will not change the sound of your voice” — not trying to offer medical advice to anyone considering or already-taking HRT. “You should ditch spiro because I have a vested interest in the concept of estrogenated power” is not the takeaway, I do want to be clear on that front! But as you say, there’s a certain degree of received wisdom that can inhibit more effective care, from even investigating the possible effects of estrogen ‘monotherapy,’ for example.
LOLA: There is a really useful concept I’ve found in repro rights discussions re: “irreversibility” that distinguishes decisional and situational regret. Are you familiar with it? Basically, as providers we are in positions to gatekeep the people we encounter making “irreversible” medical decisions (like having an abortion or starting HRT). We want to make sure that each person is doing the thing that is right for them (maximum benefit, minimum harm). In this post-irreversible-medical-procedure context, regret is not one indivisible thing but breaks down into situational regret (“I wish I hadn't needed to start T”) and decisional regret (“I should not have started T”) Situational regret is much more common than decisional regret, and also, very importantly, impossible to stop by medical gatekeeping.
Also — as we discussed at the top!!!! — unlike the decision to end a pregnancy, HRT is an incremental process made up of daily decisions to continue for as long as someone wants to do so.
DANNY: Not in those exact terms, but I have come across this concept, yes. Having a clear understanding of both the known and possible effects of whatever type of HRT one is considering is an unalloyed good! I always want to try to replace vagueness with specificity wherever possible with regards to transition, especially with transition-related fears. “I’m afraid of becoming like my father,” for example, while certainly emotionally resonant, is pretty difficult to nail down into particulars. The good news, I think, is that there is no single “turning into your father” dose of HRT; the tricky part is helping patients distinguish between what HRT does and how people (both ourselves-as-patients and the world at large) react to what HRT does.
LOLA: Turning into your father (irreversible) Expected Onset: 13-15 years. Expected Maximum Effect: Variable.



Thank you both for this. I have so much to [un]learn. Also “god’s first pancake” is the name of my new embroidery guild.